At the Bhagwan Mahaveer Cancer Hospital & Research Centre (BMCHRC), our Interventional Oncology represents the forefront of compassionate cancer care. We understand that a cancer diagnosis can be overwhelming, both physically and emotionally, which is why our dedicated team is committed to providing personalized and comprehensive care to every individual who walks through our doors.
Interventional Oncology is a branch of cancer care that uses imaging (X‑ray, ultrasound, CT, MRI) to perform pin‑hole procedures for diagnosis and treatment.
Instead of large cuts, the doctor works through tiny skin openings using fine needles and thin tubes (catheters) to reach the tumour from inside the body.
These treatments can shrink or destroy tumours, relieve symptoms like pain or jaundice, and help patients who are not fit for major surgery. They are usually done under local anaesthesia or short general anaesthesia, with faster recovery and shorter hospital stay compared to open surgery.
.webp)
Ablation means destroying a tumour from inside by heating or freezing it, without cutting it out.
Radiofrequency Ablation (RFA): Uses electrical energy to heat the tumour and kill the cancer cells.
Microwave Ablation (MWA): Uses microwave energy to create a larger and more even zone of heat, useful in liver and lung.
Cryoablation: Freezes the tumour using very low temperatures, helpful when the lesion is close to sensitive structures.
These procedures are commonly used for small cancers in the liver, kidney, lung and some bone lesions. They can provide a curative option in early disease or help control limited metastatic deposits in selected patients.
 and Embolization.webp)
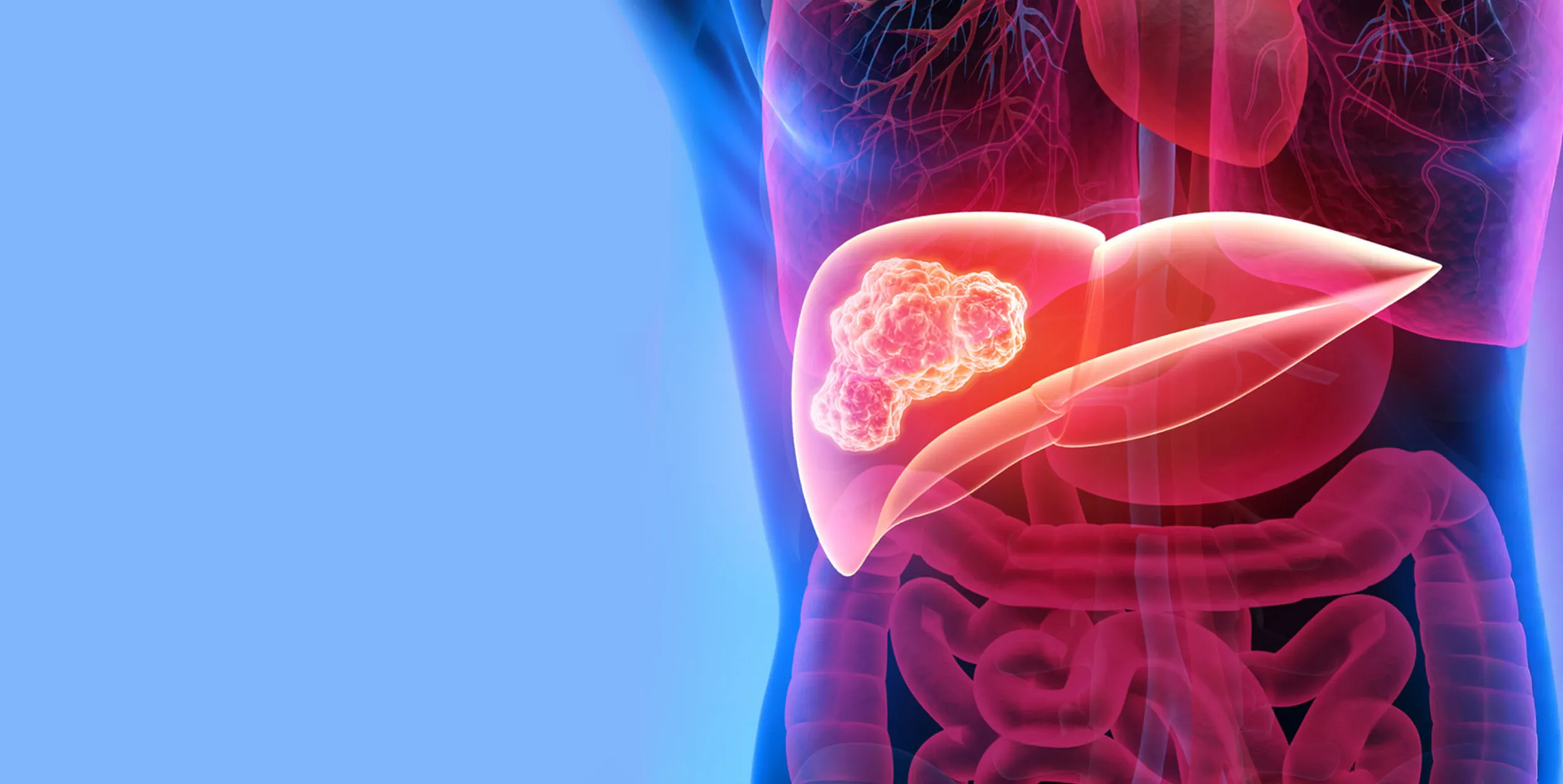
Transarterial procedures treat tumours through their blood supply.
TACE: A chemotherapy drug mixed with contrast or beads is injected into the artery feeding the tumour, followed by particles that block the blood flow. This keeps a high drug dose inside the tumour and starves it of blood.
Bland Embolization (TAE): Uses particles alone without chemotherapy to cut off the blood supply, often for tumour shrinkage or to control bleeding.
TACE is an established treatment for many patients with liver cancer who cannot undergo surgery or transplant and is often recommended in international guidelines for intermediate‑stage hepatocellular carcinoma.
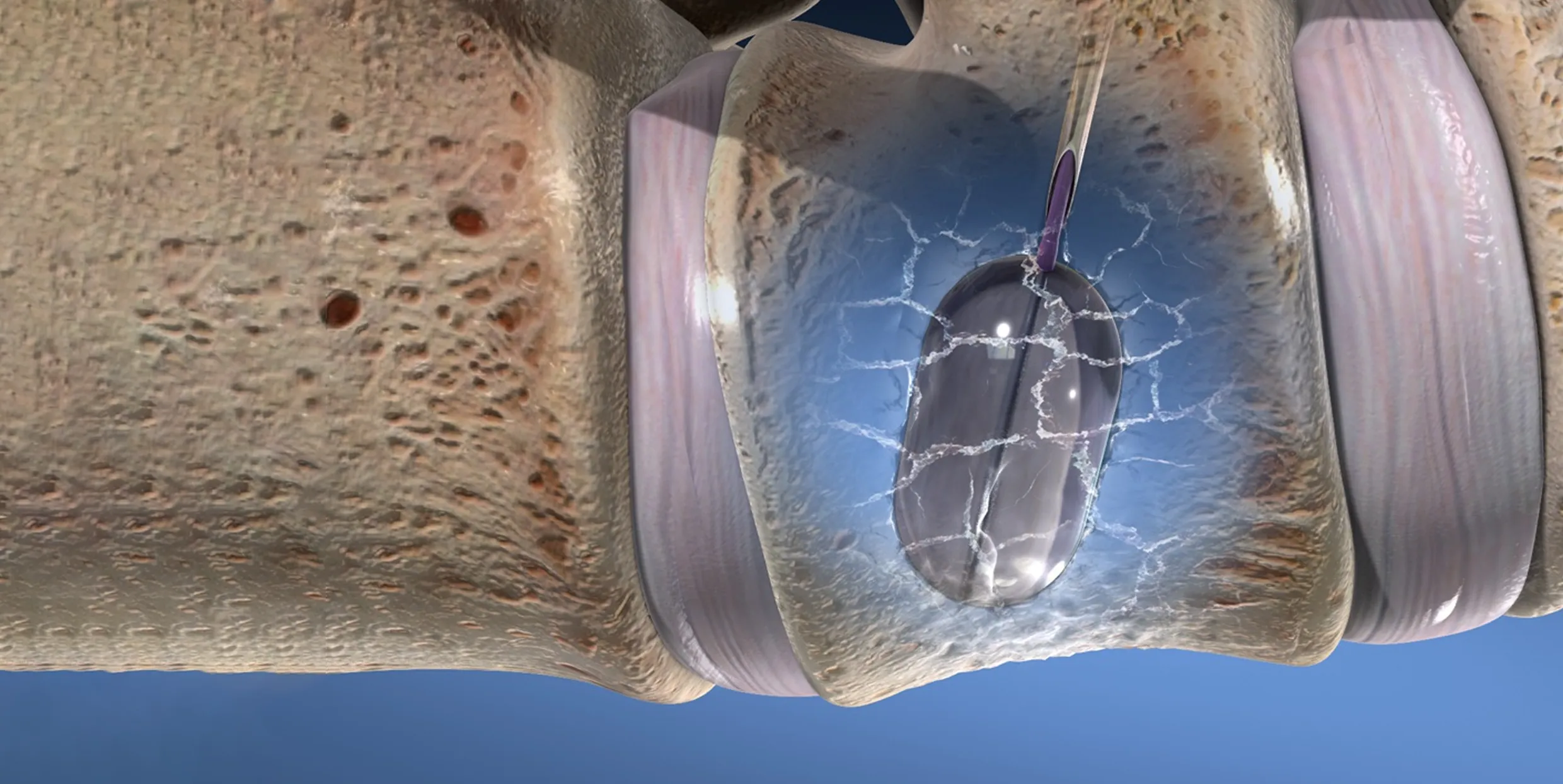
These procedures treat painful spinal fractures caused by cancer deposits or osteoporosis.
Under imaging guidance, a needle is placed into the broken vertebra.
In vertebroplasty, medical cement is injected to stabilise the bone.
In kyphoplasty, a small balloon may first be inflated to restore some height before cement injection.
Most patients experience rapid and significant pain relief, improved mobility and reduced need for strong pain medicines when carefully selected for these procedures.

For accurate diagnosis and treatment planning, a tissue sample is often essential.
Using ultrasound or CT, a fine needle is guided safely into deep or small lesions in organs such as liver, lung, bone, lymph nodes or soft tissues.
The sample is sent for histopathology and, when required, molecular or genetic tests.
This approach avoids open surgery in many cases, helps confirm the exact type of cancer, and guides targeted or immunotherapy choices.

Cancer or its treatment may lead to fluid collections or infected pockets in the body.
Common image‑guided drainage procedures include:
Pleural fluid drainage and pleurodesis for recurrent fluid around the lungs.
Ascitic and abdominal collection drainage using fine catheters.
Drainage of abscesses or post‑operative collections under ultrasound or CT guidance.
These procedures help relieve breathlessness and pain, control infection, and improve comfort with minimal trauma.

Tumours of the liver, bile ducts, pancreas or nearby lymph nodes can block bile flow and cause jaundice; pelvic or retroperitoneal tumours may block urine flow.
Percutaneous Transhepatic Biliary Drainage (PTBD): A tube is placed through the liver into the bile ducts to drain bile externally or internally.
Biliary Stenting: A plastic or metal stent is placed across the narrowing to keep the bile duct open.
Nephrostomy: A tube is placed directly into the kidney to relieve obstruction.
Antegrade ureteric stenting: A stent is placed from above when retrograde placement is not possible.
These procedures can improve liver and kidney function and allow patients to receive further systemic therapy.
Certain patients need interventions on the portal vein or major veins to make surgery safer or to relieve symptoms.
Key examples include:
Portal Vein Embolization (PVE): Blocks branches of the portal vein on one side of the liver so that the remaining liver can grow before major resection.
Venous Angioplasty and Stenting: For narrowing or blockage of major veins, such as the superior vena cava (SVC), iliac veins or IVC, which can cause swelling, breathlessness or neck‑vein congestion.
Catheter‑directed thrombolysis / thrombectomy and IVC filters: In selected patients with extensive deep vein thrombosis or high‑risk pulmonary embolism where systemic anticoagulation alone is not enough.

Interventional Oncology also plays a key role in symptom control and improving quality of life.
Nerve blocks and neurolysis (for example celiac plexus block) for severe cancer‑related pain.
Ablation and cementoplasty for painful bone metastases.
Indwelling catheters or pleurodesis for recurrent fluid collections.
These procedures are especially important in advanced disease, helping patients remain more active and comfortable.

Interventional Oncology procedures at BMCHRC are performed in dedicated imaging‑based procedure rooms designed for minimally invasive work.
Real‑time ultrasound and CT guidance is used for accurate needle and catheter placement.
High‑quality fluoroscopy systems help in vascular and biliary work.
A full range of ablation probes,stents, drainage catheters and bone cement systems is available as per clinical need.
Strict protocols are followed for infection control, radiation safety and monitoring during and after each procedure.
Small incisions, big impact: Many procedures are done through needle punctures, leading to less pain, fewer complications and quicker recovery.
Option for high‑risk patients: Suitable for many patients who are elderly, frail or not fit for major surgery.
Targeted treatment: High concentration of therapy at the tumour site, often with fewer whole‑body side effects.
Works with other treatments: Can be combined with chemotherapy, targeted drugs, immunotherapy, surgery and radiation for better overall control.
Focus on comfort and quality of life: Strong role in pain relief and symptom control at all stages of cancer.
Interventional Oncology uses scans (Like Ultrasound, CT or X‑Ray) to guide thin needles and catheters inside the body to diagnose or treat Cancer through tiny skin openings. It is one of the main pillars of modern Cancer Care, along with medical, Surgical and Radiation Oncology.
Traditional Surgery usually needs larger cuts and longer recovery. Interventional Oncology procedures are Minimally Invasive, so most patients have less pain and shorter hospital stay. Chemotherapy travels throughout the body in the bloodstream, whereas many interventional treatments act mainly at the tumour site, so they can sometimes use higher local doses with fewer whole‑body side effects.
Every medical procedure carries some risk. However, these treatments are designed to reduce trauma by using small punctures, careful imaging and strict safety checks. Possible risks depend on the procedure and may include bleeding, infection, contrast reaction or damage to nearby organs. The doctor will explain the expected benefits and specific risks in your case before you consent.
Most procedures are done under local anaesthesia, sedation or general anaesthesia, so patients are usually comfortable during the procedure. Some temporary pain or discomfort can occur afterwards, such as shoulder pain after liver ablation or back soreness after vertebroplasty, but this is usually short‑lived and controlled with medicines.
This depends on the type of procedure and your overall health. Many biopsies, drainages and some ablations or vertebroplasties are done as day‑care or overnight stay. Liver‑directed treatments like TACE or complex vascular procedures may require 1–3 days of observation. A longer stay may be needed if you have other medical problems or if the procedure is combined with surgery or intensive chemotherapy. Your doctor will inform you about the expected duration in advance.
“Success” may mean different things: complete tumour kill, slowing down growth, relieving pain, or improving organ function. Results depend on tumour size, number, location, stage, previous treatment and your general condition. For carefully selected patients, ablation and liver‑directed therapies can provide good local control and improved survival compared with best supportive care alone.
Yes. These procedures are often part of a combined plan—for example:
Preparation usually includes:
Most patients can start moving early, often on the same or next day. Mild tiredness, low‑grade fever or reduced appetite can occur after some procedures, particularly liver‑directed therapies, but these usually settle in a few days with simple medicines and rest. Follow‑up visits and scans are important to check the effect of treatment and plan further care if needed.
Yes. Patients and families are encouraged to ask questions and seek a second opinion if they wish. The team at BMCHRC supports open discussion, explains all suitable options and helps you choose a plan that matches your values, expectations and overall health.
Request a callback from our healthcare specialist